What is sterilization validation?
Medical device sterilization validation ensures that sterilization processes reliably eliminate microorganisms to a safe level, typically achieving a Sterility Assurance Level (SAL) of 10⁻⁶, meaning a one-in-a-million chance or less of a single, viable microorganism surviving on a device. This process is critical for patient safety and regulatory compliance.
Validation begins with selecting an appropriate sterilization method, such as ethylene oxide (EO) or a form of radiation, based on material compatibility. It includes assessing bioburden (microbial load) to determine “how much” sterilization is required. Tests then determine effective sterilization parameters: e.g. dose in radiation sterilization or process parameters for EO.
Key steps also include ensuring material compatibility, testing packaging integrity, and monitoring residuals like EO gas. Validation adheres to standards like ISO 11135 and ISO 10993-7 (EO) and ISO 11137 (radiation), requiring routine review of process performance and periodic requalification to maintain process effectiveness.
By validating sterilization, manufacturers ensure medical devices are sterile, functional, and meet global safety standards, safeguarding patient and healthcare provider health.
What are the key differences between EO and radiation validations?
Validation approaches differ due to the nature of each modality. A summary is below:
| Category | EO | Radiation |
|---|---|---|
| ISO Standard | 11135 and 10993-7 | 11137 |
| Mechanism of Pathogen Kill | Alkylation via penetrative toxic gas | Ionizing radiation |
| Process Development | Involves parameters like load configuration, gas concentration, temperature, humidity, and exposure time. Sterilization validation can be based on bioburden, biological indicators, or overkill methods. | Sterilization validation is bioburden-based, focusing on bioburden testing to establish the sterilization dose and dose mapping for uniformity. |
| Residuals | Leaves potentially carcinogenic chemical residuals (e.g., ethylene oxide gas and by-products like ethylene chlorohydrin), requiring post-sterilization aeration to meet safety standards. | None. |
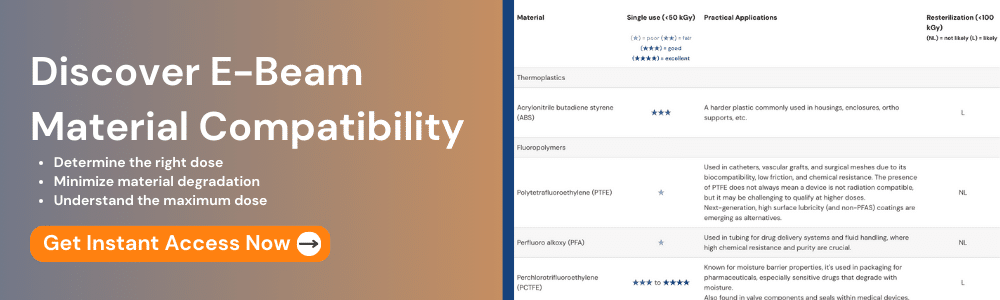
| Material Compatibility | Suitable for delicate and radiation-sensitive materials, such as certain electronics and polymers. Not suitable for materials sensitive to humidity or that react with EO. | Works well for many materials but may degrade certain plastics, elastomers, or pigments. Of radiation technologies (Gamma, E-beam, X-ray), E-Beam is typically gentlest on materials due to rapid dose delivery. |
Time, Money, Risk: How do the methods compare?
For each method, both the speed and amount of product being processed in parallel tend to drive the time and cost associated with validation:
EO
- At scale, EO is a massively parallel batch process with many pallets placed in a large, airtight chamber, where they are gassed.
- Cycles can last from 1-4 days and are done in full-scale production chambers, requiring providers to schedule these assets in advance for cycle development, and pacing the overall validation
- Validations with practical scale tend to be significantly more expensive (more test product is required – enough to define the maximum routine load configuration)
Radiation
- Process design varies by modality. E-Beam / X-ray (together, “accelerator-based modalities”) are (mostly) serial processes where products are typically dosed in seconds to minutes. Gamma irradiation is a more parallel process where products are typically dosed over hours.
- Validations tend to be less expensive (even a very large scale process requires the same minimal amount of product to validate, and does not require the same amount of beam time as a full batch.)
| Category | EO | Radiation |
|---|---|---|
| Time | Typically 3-6 months (large variation due to lack of validation capacity) | Typically 6-8 weeks |
| Money | Wide variation ($10,000 - $100,000) with larger chambers costing more | Typically ~$20,000 |
| Risk |
Litigation risk: hundreds to thousands of lawsuits have been filed against EO facilities over the past decade. Legal fees, increased regulation, and reduced competition will drive up costs. |
Accelerator-based modalities: facility can have unexpected downtime (typically short duration). Gamma: lack of Cobalt-60 can cause major price increases and lack of capacity. |
We have previously written in greater detail on how both processes compare in terms of schedule and cost
Living with Validated Processes
Once a sterilization process is validated, there are ongoing monitoring requirements for each, as specified in ISO 11135 and 11137 standards. The unique nature of each modality means that the maintenance requirements are different, however.
Both processes also have their critical process parameters monitored continuously (for EO, key metrics include pressure, temperature, humidity, gas concentration) For accelerator-based radiation: beam current, energy, conveyor speed, etc are monitored.
Some EO processes include biological indicators (BIs) that are included in each process in addition to monitoring of physical parameters.. In contrast, radiation-based modalities rely on dosimetry (the measurement of radiation dose) to assure that the process was correctly executed. Both methods require that sterilization providers have specialized lab capabilities to assess on a daily basis.
As an additional check on radiation-based methods, dose audits are performed using low doses to monitor the radiation resistance of the product bioburden over time, typically quarterly.
How It Breaks Down
EO is a very high performance sterilization modality – and medical device products often can require it because their materials are fundamentally not radiation compatible (though, more and more, we see that there are better options for increasing material compatibility). However, in these cases, the increasing cost of EO and its other associated risks (e.g. litigation) must be accounted for.
Radiation, on the other hand, especially via accelerator-based modalities, is a highly scalable, environmentally-friendly process that is highly mature and cost effective – and this begins with the higher speed and lower cost of establishing and maintaining sterilization validations.
We are always available for free consultations on sterilization validation methods. Contact us today if we can be of service.
Additional Articles We Think You Might Like
Have a question? Speak with a sterilization expert today, at your own convenience.