Sterility is critical to ensuring the safety and efficacy of medical devices, particularly those intended for invasive use. The Sterility Assurance Level (SAL) represents the probability of a single viable microorganism surviving after sterilization. Selecting the appropriate SAL is a key decision for medical device manufacturers and must balance regulatory compliance, patient safety, and product functionality.
Here’s how manufacturers can effectively choose the right SAL for their devices.
Understanding SAL
The SAL is expressed as a negative exponent, such as 10-6 or 10-3, representing the probability of one surviving microorganism per 1,000,000 or 1,000 sterilized items, respectively. Higher SALs (e.g., 10-6) indicate stricter sterility standards, historically associated with more invasive applications, while lower SALs may suffice for less invasive applications.
Key Considerations for Selecting SAL
1. Device Classification and Use
The primary factor in determining SAL is the device’s intended use and contact with the body. Regulatory agencies, including the FDA and ISO 11737-2 standards, provide guidelines based on device classification:
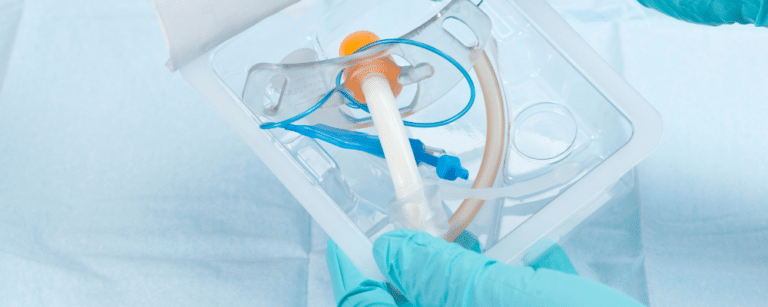
- Critical devices (e.g., implants, surgical instruments) require an SAL of 10-6 due to direct contact with sterile body sites or blood.
- Semi-critical devices (e.g., endoscopes) may require an SAL of 10-3, as they contact mucous membranes rather than sterile tissue.
- Non-critical devices (e.g., external cables or sensors) can require sterilization if used in a sterile field, or might only be disinfected under lower risk conditions.
2. Risk Assessment
Manufacturers should conduct a thorough risk assessment to evaluate potential infection risks posed by microorganisms. This includes considering:
- Possible sources of microbes present in the manufacturing process: raw materials, manufacturing environment, in process materials (machining fluids, coatings), personnel.
- Consequences of infection in the intended patient population.
- Any cleaning steps during or at the end of the manufacturing process
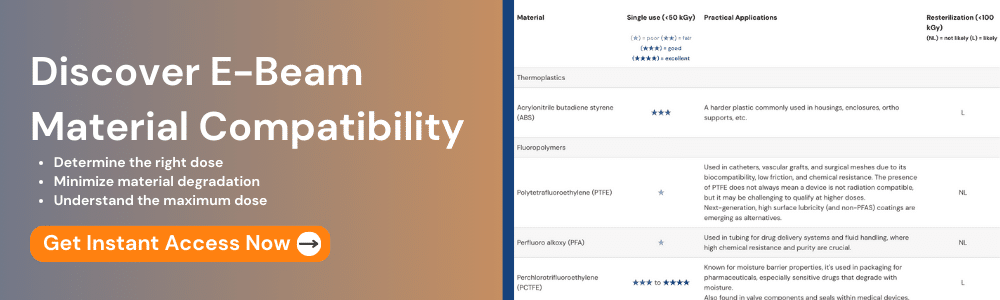
3. Material Compatibility
Materials compatibility is usually the first question that comes up when selecting a sterilization technology. For example:
- Radiation technologies, e.g. gamma, E-beam, X-ray, can penetrate certain design features and packaging configurations that are inaccessible to gas sterilization technologies, such as foil pouches or impermeable hermetically sealed features. However, radiation can affect mechanical properties of many polymers in a positive or negative manner, which has to be managed by carefully setting the maximum permissible dose and avoiding incompatible materials.
- Gas technologies such as EO or VHP are compatible with a wide range of materials including polymers, with exceptions for materials that are impermeable or react with the sterilant such as some hydrophilic coatings or organic materials.
Understanding how the chosen sterilization process aligns with the device material and design is essential.
4. Regulatory and Market Requirements
Regulatory standards differ by region and device type. Manufacturers should ensure that their chosen SAL complies with the most stringent requirements applicable to their target markets as there can be differences in required SAL between US, EU, and other countries.
Optimizing SAL Selection
To balance sterility and product integrity, manufacturers should:
- Engage early with sterilization experts to evaluate methods and SAL requirements.
- Validate sterilization processes with comprehensive testing to confirm SAL effectiveness and materials compatibility.
- Document decisions thoroughly to demonstrate compliance with regulatory standards during audits.
Conclusion
Selecting the appropriate SAL is a nuanced decision that requires a deep understanding of device use, risks, materials, and regulatory expectations. By carefully evaluating these factors and adopting robust validation practices, medical device manufacturers can ensure patient safety, regulatory compliance, and product performance. At NextBeam we work with customers every day to ensure our tailored sterilization processes provide appropriate safety levels and risk reduction are delivered, along with optimal processing efficiency and economics. Please contact us for a free consultation!
Additional Articles We Think You Might Like
Have a question? Speak with a sterilization expert today, at your own convenience.